October 1, 2012, marked the beginning of the Hospital Readmissions Reduction Program (HRRP), an ambitious effort by the Centers for Medicare and Medicaid Services (CMS) to reduce the frequency of rehospitalization of Medicare patients. The program consists primarily of financial penalties levied against hospitals with readmission rates that are deemed to be excessive. To assign penalties, CMS calculated expected readmission rates for all hospitalizations for acute myocardial infarction, congestive heart failure, and pneumonia from July 2008 through June 2011, adjusting for age, sex, and coexisting conditions such as diabetes and hypertension. These expected rates were then compared with the actual readmission rates over the same period, and penalties were assessed against hospitals whose observed rate exceeded the expected rate. According to CMS, approximately two thirds of U.S. hospitals will receive penalties consisting of up to 1% of their reimbursement for Medicare patients; these penalties will increase to 3% by 2015. CMS expects to recoup $280 million from the 2217 hospitals penalized in 2013 alone.
Penalizing hospitals for high readmission rates has been controversial since the idea was introduced, with criticism primarily focused on two main areas. The first point of contention is whether the hospital is the appropriate entity to be held accountable for readmissions, given that the events and circumstances that predict readmissions largely take place outside the hospital’s walls. The second set of concerns is focused on the specific attributes of the measure itself. There is overwhelming evidence that two groups of patients are at particularly high risk for readmissions: those who have the most severe illnesses (because of their underlying condition) and those who are socioeconomically disadvantaged 1 (probably because they lack access to important resources after discharge, such as social support or primary care).
The current measure does not take important measures of severity of illness such as disability and complexity into account, and it opts out of accounting for socioeconomic status altogether, leaving hospitals that disproportionately care for the sickest and poorest patients at particular risk for penalties.
Two developments over the past year have provided new insights into how the program is playing out and may lead to guidance for improving it. The first was a report from the Medicare Payment Advisory Commission indicating that there has been a small but significant decrease in national rates of readmission for all causes, from 15.6% in 2009 to 15.3% in 2011. 2 The HRRP has generated an immense amount of readmissions-prevention activity in U.S. hospitals, and these efforts appear to be having a beneficial effect. Although it is possible that the small reductions in readmissions rates are caused by gaming of the system (e.g. more patients being held in emergency departments or admitted for observation) or that the gains are transitory, we are hopeful that the modest decrease in readmission rates represents real gains in care that will be sustained over time.
The second important development was the release of data on who will be penalized: two thirds of eligible U.S.
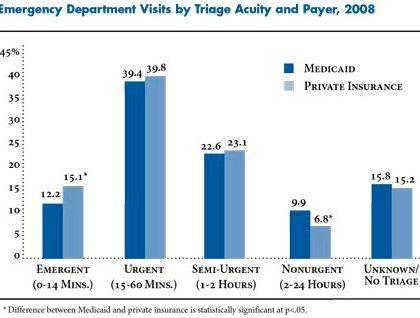
hospitals were found to have readmission rates higher than the CMS models predicted, and each of these hospitals will receive a penalty. The number of hospitals penalized is much higher than most observers would have anticipated on the basis of CMS’s previous public reports, which identified less than 5% of hospitals as outliers. In addition, there is now convincing evidence that safety-net institutions (see graphs Proportion of Hospitals Facing No Readmissions Penalty (Panel A) and Median Amount of Penalty (Panel B), According to the Proportion of Hospital’s Patients Who Receive Supplemental Security Income. ), as well large teaching hospitals, which provide a substantial proportion of the care for patients with complex medical problems, are far more likely to be penalized under the HRRP. 3 Left unchecked, the HRRP has the potential to exacerbate disparities in care and create disincentives to providing care for patients who are particularly ill or who have complex health needs, particularly if the penalties are larger than hospitals’ margins for caring for these patients.
Given these two new insights, we believe that there are several steps that could be taken to sustain the gains that have been achieved while avoiding substantial harm to hospitals that care for the most socially and clinically vulnerable patients. First, adjusting readmission rates for socioeconomic status — for example, by adding patients’ eligibility for Supplemental Security Income to the risk-adjustment models — could help put hospitals on a level playing field. If readmissions were a straightforward measure of quality (e.g. the use of aspirin for acute myocardial infarction), such an adjustment would be inappropriate — no one wants to give hospitals credit for providing bad care to poor patients. However, insofar as data on readmission rates primarily capture the socioeconomic and health status of patients 1 rather than hospital quality, 4 adjusting for socioeconomic status would ensure that if a safety-net hospital can achieve similar readmission rates as non–safety-net hospitals for its poor patients, having an additional number of poor patients would not, in and of itself, lead to penalties, as it does now.
Second, weighting the HRRP’s penalties according to the timing of readmissions might improve the algorithm. Readmissions that occur within the first few days after discharge may reflect poor care coordination or inadequate recognition of postdischarge needs, whereas readmissions 4 weeks later are far more likely to be due to the underlying severity of a patient’s disease. When a readmission occurs 3 hours or 3 days after discharge, it could be weighed more heavily than a readmission that occurs 30 days after discharge. Under such a scheme, hospitals that care for sicker or more socioeconomically vulnerable populations could still make improvements to discharge planning and care coordination to prevent short-term readmissions without being penalized for the fact that their patients generally have more complex medical conditions and social situations and are therefore more likely to need additional hospital services over the long run.
Finally, giving hospitals credit for low mortality rates would acknowledge the competing risks at play in the readmissions metric. Hospitals with a low mortality rate among patients with heart failure, for example, tend to have higher readmission rates, although this relationship is not consistent across conditions. 5 It would make sense if high-performing hospitals that kept their sickest patients alive were not penalized if some patients who would otherwise have died were readmitted. Factoring a hospital’s mortality rate into its readmission-penalty calculation could ensure that the best institutions (those with the lowest mortality rates — often large teaching hospitals) were not inappropriately penalized. As things stand, hospitals with high mortality rates but low readmission rates do better under the CMS payment scheme than hospitals with low mortality rates but high readmission rates. One method by which these two outcomes could be combined is to assess patients’ 30-day “days alive and out of hospital.”
No policy is ever perfectly designed at inception, and policies should be changed as new evidence emerges. The latest evidence suggests that the readmissions-reduction program has potential: it can change the hospital business model by asking institutions to become increasingly accountable for what happens to their patients beyond their walls. Over time, hospitals can become an organizing entity for more coordinated, efficient care. These would be good things for patients and for the health care system at large. However, the latest data also make it clear that the HRRP will penalize hospitals that care for the sickest and the poorest Americans, largely because readmissions are driven by the severity of underlying illness and social instability at home. Simple changes to the program could ensure that incentives were provided to hospitals to improve coordination of care without hurting the institutions that care for the most vulnerable patients.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
This article was published on March 6, 2013, at NEJM.org.






 Catchy titles for feature articles and writing
Catchy titles for feature articles and writing Best online article writing sites
Best online article writing sites Writing newspaper articles ks3 english
Writing newspaper articles ks3 english Newspaper article writing guidelines essay
Newspaper article writing guidelines essay Feature article sample topics for technical writing
Feature article sample topics for technical writing