Pre service and publish service Adverse Determination Appeals
Adverse Determination Appeals
A service provider may file an itemized request with BCBSF for reconsideration of the denial of payment just because a
suggested, or actual, healthcare service or supply wasn’t medically necessary, was experimental or
investigational, was supportive of the experimental or investigational, or was supportive of the not medically
necessary procedure (“Adverse Determination Appeal”). A Bad Determination Appeal could be of
pre-service claims or perhaps a publish-service claim when the needs outlined here are met. A Bad
Determination appeal should be on paper and isn’t triggered by claim status demands or telephone
queries regarding the use of benefits or permitted amount.
Pre-Service Adverse Determination Appeals
A health care provider (i.e. Medical Physician or Physician of Osteopathy) or physician group can appeal a pre-service
Adverse Determination (Pre-Service Appeals), if they’re appealing with respect to a BCBSF member.
Aside from urgent Pre-Service Appeals, authorization should be acquired in the BCBSF member in
writing. Pre-Service appeals is going to be handled by BCBSF underneath the appeal process open to its member
in line with the relation to that member’s contract or policy and also the relevant condition and federal laws and regulations and
rules.
A service provider can appeal a publish-service Adverse Determination (Publish-Service Appeal). A Bad
Determination Publish-Service Appeal should be posted on paper within twelve months of date of payment and
delivered to the address below using the following information:
• The finished Provider Appeal Form (offered at world wide web.bcbsfl.com).
• A duplicate from the remittance advice.
• The required medical documentation (e.g.
operative report, physician orders, background and physical)
as shown by the reason behind the reduction or even the denial around the remittance advice.
The company or provider group might not initiate an interior Publish-Service Benefit of any denied service or
supply if:
• BCBSF’s member (or their representative) or even the provider or provider group filed a Pre-Service
Appeal relating towards the same denied service or
• BCBSF’s member (or their representative) is presently seeking or has searched for an evaluation or filed
litigation associated with exactly the same denied service. In case both BCBSF’s member (or their
representative) and also the provider or provider group seek review of the identical denied service, BCBSF’s
member appeal shall move forward and also the provider or provider group appeal is going to be ignored.
Send Adverse Determination internal attracts:
Blue Mix and Blue Shield of Florida
Provider Disputes Department
P.O. Box 44232
Jacksonville, FL 32231-4232



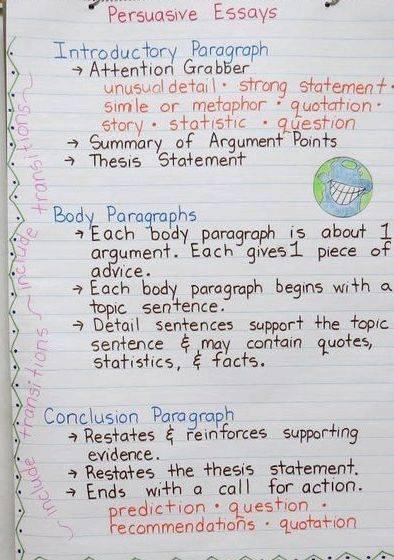

 Essay writing service singapore mrt
Essay writing service singapore mrt Essay writing service australia reviews security
Essay writing service australia reviews security Online editing services writing a check
Online editing services writing a check Resume writing service in chicago
Resume writing service in chicago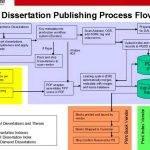 University of michigan dissertation publishing service
University of michigan dissertation publishing service