New User Registration
Not Registered Yet?
Advantages of Registration Include:
- A Distinctive Account that will help you to manage your present subscriptions (including online access)
- The opportunity to create favorites lists lower towards the article level
- The opportunity to personalize email alerts to get specific notifications concerning the topics you care most about and special deals
You’ve requested the next article:
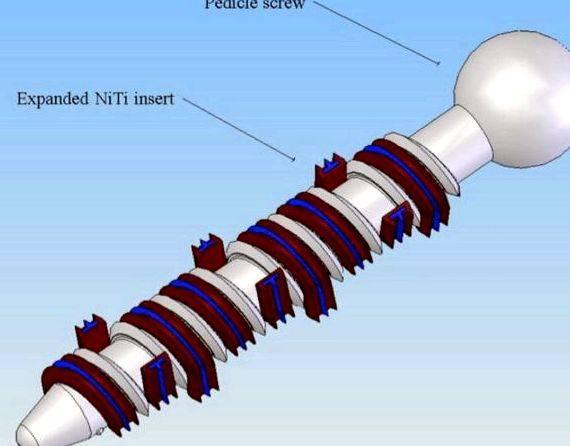
Precision of pedicle screw placement within the lumbosacral spine using conventional technique: computed tomography postoperative assessment in 102 consecutive patients
Vincenzo Amato, Luigi Giannachi, Claudio Irace, Claudio Corona,
Journal of Neurosurgery: Spine, March 2010 / Vol. 12 / No. 3. Pages 306-313
The aim of this research was to look for the incidence of screw misplacement and complications in several 102 patients who went through transpedicle screw fixation within the lumbosacral spine with conventional open technique and intraoperative fluoroscopy. The outcomes are in contrast to printed data.
Cases involving 102 consecutive patients (424 placed screws) were reviewed. Surgery was performed in every case through the same surgeon’s team, utilizing the same implant, and all sorts of outcome was assessed using a specific CT protocol. The screw position was assessed through the authors as well as an independent observer. Screw position was considered correct once the screw was completely encircled through the pedicle cortex, as “cortical encroachment” (questionable breach) when the pedicle cortex couldn’t be visualized, so that as “frank penetration” once the screw was outdoors the pedicular limitations. Frank transmission was further subdivided as minor (once the fringe of the screw thread was as much as 2. mm outdoors the pedicle cortex), moderate (2.1–4 mm), and severe ( 4 mm).
The incidence of intra- and postoperative complications not associated with screw position in addition to hardware failures were also registered, having a minimum follow-up time period of 8 several weeks.
The speed of frank pedicle screw misplacement was 5%. The speed of minimal or questionable pedicle wall breach was 2.8%. One of the frank misplacements, 6 were considered minor, 12 as moderate, and three as severe transmission. Two patients (2%) had radicular discomfort and nerve deficits (inferomedial and inferolateral minor misplacement at L-4 and L-5, correspondingly), and 5 patients (4.9%) complained only of radicular discomfort. In the follow-up examination all patients had completely retrieved their nerve function and radicular discomfort was resolved in every case. The complications not associated with screw malposition were 2 pedicle fractures (2% of patients), 1 nerve root injuries (1%), and 1 dural laceration (1%). Five patients (4.8%) had postoperative anemia and needed transfusions. Superficial or deep wound infection was noted in 3 patients (2.9%). Late hardware failure happened by 50 percent patients (2%). One patient developed adjacent segmental instability and needed additional surgery to increase the fusion.
Our rates of screw misplacement and complications compare favorably using the cheapest rates from the series by which conventional technique was utilized and therefore are near to the rates reported for image-led methods.
The chance of malpositioning might be reduced with careful preoperative surgical planning, accurate understanding from the spine anatomy, surgical experience, and proper indication for conventional surgery. The traditional technique still remains an operating, safe, and efficient surgical way of lumbosacral fixation.
Register
For those who have a person subscription for this content, or you have obtained the information through Pay Per Article in the past 24 hrs, you will gain access by signing in together with your password here:
If you are a print subscriber and haven’t activated your access, or need assistance, please send us an email at subscriptions@thejns.org
Plain X-radiographs, computed tomography (CT) scans and magnetic resonance imaging (MRI) were acquired to be able to determine the kind of fracture, the compression ratio of spine canal, whether there is an injuries of posterior ligamentous complex (PLC), etc. [ 4 ]. Thoracolumbar injuries classification and severity scores (TLICS) [ 5 ] of cases were calculated. Each patient received plain X-radiographs 2 days after surgery. CT scans were additionally a necessity if there was apparent compression of spine canal before surgery.
The procedures adopted were in compliance using the ethical standards from the responsible committee on human experimentation (institutional and national) along with the Helsinki Promise of 1975, as revised in 2000.
Description of percutaneous fixation surgery
Just one shot of antibiotics was administered pre-operatively. Under general anaesthesia with endotracheal intubation, each patient was positioned prone on the Jackson operating table. Chest and pelvis were based on gel pads fixed up for grabs. Postural reduction was performed before surgery. Lateral fluoroscopy was taken with the objective of figuring out the effectiveness of postural reduction. Posteroanterior (PA) fluoroscopy was utilized to find one level above and underneath the hurt vertebra. The related positions of pedicles were marked around the patient’s back. After undergoing disinfection from the surgical area, skin incisions were created 1.5-cm lateral in the marks of individuals pedicles. Underlying fascia was cut by an electrosurgical knife and paraspinal muscles were split with a finger. Under PA fluoroscopy, each pedicle was cannulated with a Jamshidi needle in the lateral and medial margin. The insertion directions were adjusted based on lateral fluoroscopy. The needle ended up being gradually implanted via a pedicle. Via PA notice is made certain each needle wasn’t passed over the medial border from the corresponding pedicle, which recommended that there wasn’t any breach of spine canal. A guidewire was put into the vertebral body with the needle, adopted by consecutive dilators that could safeguard paraspinal muscles while developing a space for tapping. The dilators were then removed, allowing a percutaneous pedicle screw to become placed in to the pedicle and vertebral body across the wire that was also brought out right after. Each percutaneous pedicle screw was placed right into a pedicle along with a vertebral body in the same manner. The adjacent amounts of fractured vertebra were implanted with bilateral pedicle screws in group B while yet another set of screws were implanted in to the fractured vertebra in group A. Therefore, there have been six percutaneous pedicle screws implanted into each patient’s thoracolumbar region in group A (Fig. 1d, e ) and 4 screws in group B (Fig. 2d, e ). The size of rods was assessed based on the distance between cranial and caudal screws. An appropriately bent fishing rod was put into the screws’ heads of 1 side underneath the fascia. The peak of fractured vertebra was further restored by making use of a hyperlordosing pressure with the posterior elements right before the group of screws were tightened. Exactly the same procedure was adopted on the other hand. Good location of internal fixation and acceptable correction of kyphosis were confirmed by PA and lateral fluoroscopy. Finally, incisions were irrigated and closed layer-by-layer without drainage.
Images from the 35-year-old female in group A. a. b Preoperative radiographs indicating a fracture of T12. c. d Publish-operative radiographs indicating favorable restoration of anterior height of T12 vertebra and correction of Cobb position
Images from the 43-year-old male in group B. a. b Pre-operative radiographs indicated a fracture of L1. c. d Publish-operative radiographs indicated favourable restoration of anterior height of L1 vertebra and correction of Cobb position
Description of open fixation surgery
Dose-appropriate antibiotics were also administered in the induction. General anaesthesia and endotracheal intubation were conducted within the same means by group A and group B. Postural reduction and skin disinfection were also performed inside a prone position for patients in group C on the Jackson operating table prior to the surgical treatment. After posterior thoracolumbar elements were clearly uncovered with the traditional posterior approaches, the fractured and adjacent vertebrae were implanted with as many as six pedicle screws by free hands. Appropriately sized rods were put into screws’ heads and kyphosis was remedied with a hyperlordosing pressure. Subsequently, locking screws were tightened (Fig. 3d, e ). Irrigation from the cut was frequently performed and drainage was placed before individuals layers were strictly closed. Generally, drainage was removed within 48 hrs following the surgical treatment.
Image from the 38-year-old male in group C. a. b Pre-operative radiographs indicated a fracture of L2. c. d Publish-operative radiographs indicated favourable restoration of anterior height of L2 vertebra and correction of Cobb position
Within the pre- and publish-operative period, all patients were asked to do muscle flexing of lower braches with the objective of staying away from muscle atrophy and reducing the chance of deep venous thrombosis. Each patient in group A and group B was asked to have ambulatory activities while putting on a thoraco-lumbar-sacral brace 72 hours after surgery. The beginning duration of ambulatory activities for patients in group C was two days publish-operatively. All patients commenced back muscle exercises a week after surgery. The brace was stored until three-month follow-up. Neither sports nor strenuous work was permitted within six several weeks after surgery. Plain X-radiographs were acquired at 30 days, three several weeks, six several weeks, twelve months and 2 years publish-operatively. All patients recognized surgery of instrumentation removal throughout six several weeks to 1 year when plain X-radiographs confirmed good healing of fractured vertebra.
The next radiological data were collected. Anterior height ratios (AHR) of fractured vertebrae and Cobb angles (CA) (Fig. 4 ) were measured in pre- and postoperative plain X-radiographs (Figs. 1. 2 and 3b, e ). The anterior height ratio of the fractured vertebra was calculated by dividing the anterior height from the fractured vertebra by its normal height. And also the normal height of the fractured vertebra was believed if you take the typical between your anterior heights of lower and upper adjacent vertebrae. A Cobb position was measured between your superior endplate from the upper vertebra and also the inferior endplate from the lower vertebra. A correction loss was calculated by subtracting the Cobb position of ultimate follow-up in the first publish-operative one.
Cobb position (CA) and native sagittal position (LSA)
Clinical parameters was comprised of time period of surgery, intra-operative bloodstream loss and visual analogue scale (VAS). VAS scores, assessing the magnitudes of patients’ back discomfort, were measured at pre-operative time, three several weeks follow-up and also the final follow-up.
Record analysis methods
All radiological and clinical data were examined by utilizing SPSS record package, version 16. (SPSS, Chicago, IL, USA). Chi-square test was utilized for analyzing categorical data among three different groups. Continuous variables were recorded because the mean ± SD. Among-group comparisons were created using ANOVA. If there is record significance, between-group comparisons were created by performing Dunnett-t test. For every analysis, a P worth of .05 was considered statistically significant.
Results
The typical follow-up was 17.7 several weeks (range 11–25 several weeks). There wasn’t any factor in baseline demographic characteristics among three groups (p .05) (Table 1 ). No significant among-group difference concerning pre-operative VAS score, Cobb position or anterior height ratio of fractured vertebra was observed (p .05). No nerve complication was noted. One situation in group A who was simply diagnosed as diabetes endured from publish-operative wound infection four days after surgery. The problem was soon controlled after treatments, including irrigation, debridement and rational utilization of antibiotics, without removing internal fixation. Screw loosening was noticed in one situation in group B at three several weeks without any clinical symptom. The individual was recommended to lessen ambulatory activities, increase back muscle exercises and putting on a brace before the time when good healing from the fracture was confirmed. The instrumentation from the patient was removed six several weeks following the first surgery, and also the effects were favourable in the final follow-up.
The typical durations of surgery in group A, group B and group C were 72.1 ± 12.5 min, 64.4 ± 9.8 min and 77.8 ± 8.2 min, and also the values of intra-operative bloodstream loss were 100.7 ± 18.9 ml, 89.1 ± 17.3 ml and 202.1 ± 42. ml, correspondingly. Time period of surgery was considerably shorter in group B than group A (p .05). There wasn’t any factor concerning time period of surgery between group A and group C (p = .068). The of intra-operative bloodstream reduction in group A were considerably under individuals in group C (p .05). VAS scores for back discomfort at three several weeks after surgery were 2.2 ± .5, 2.4 ± .5 and three.3 ± .5 points in group A, group B and group C. The scores in group A were considerably less than individuals in group C (p .05). The main difference between group A and B wasn’t statistically significant (p = .612) (Table 2 ).
Clinical parameters (group A versus group C)
CA Cobb position, AHR anterior height ratio
Discussion
The greatest incidence of spine fractures happened in the thoracolumbar region due to its special physiological features [ 6 ]. It’s belief that a vertebral height loss in excess of fifty percent, a nearby sagittal position (LSA) (Fig. 4 ) in excess of 20 levels or posterior ligamentous complex (PLC) injuries might be unstable findings for traumatic thoracolumbar fractures [ 7 ]. Type A thoracolumbar fractures are without PLC injuries. Both conservative management and surgical intervention are recommended [ 8. 9 ]. Surgical fixation provides not just better fracture reduction, but additionally initial stability which helps early mobilization. Thus, it may effectively decrease complications connected with prolonged recumbence [ 1. 7 ]. Even though the connection between traditional open surgery for patients who’d indications are usually favourable, the extensive harm to soft tissue unavoidably produces a relatively high incidence of unsuccessful back surgery syndromes [ 10. 11 ]. Using the rapid growth and development of non-invasive approaches for spine recently, percutaneous pedicle screw fixation has acquired its recognition since the method has an apparent advantage in protecting paraspinal muscles from iatrogenic denervation and atrophy. Lee et al. [ 12 ] noticed that in comparison with conventional posterior surgery, the present non-invasive procedure had benefits of costing less surgical treatment-related trauma and making certain earlier recovery. The outcomes of the study also demonstrated the values of intra-operative bloodstream reduction in percutaneous fixation groups were considerably under individuals on view fixation group. Patients who went through non-invasive surgery had lower publish-operative VAS scores at three-month follow-up, which signifies that back discomfort is correctly connected using the harm to paraspinal muscles on view surgical treatment. Besides, patients within the percutaneous fixation group are permitted to possess ambulatory activities much earlier, and will also be less uncovered to complications of bed rest [ 13 ].
Within the study, there wasn’t any factor concerning kyphosis correction between three-level percutaneous fixation and three-level open fixation. Even though the current non-invasive fixation method has a lot of advantages, it’s still at its initial phase. Inevitably, disadvantages, including more contact with radiation and greater amount of complications with fracture reduction can’t be overlooked. However, such disadvantages are unquestionably likely to be reduced or perhaps be prevented by the introduction of technology concerning spine surgery navigation, automatic guidance and so forth [ 14 ].
Before the use of minimally percutaneous fixation procedure, the thought of placing pedicle screws at the amount of the fractured vertebra, causing considerable debate, was suggested by a few authors. They considered the reduction procedure with short segment fixation across fractured vertebra, or named two-level fixation, to become indirect. Furthermore, a greater proportion of instrumentation failure along with a bigger amount of correction loss were noticed in patients with two-level fixation. In 1994, Dick et al. [ 15 ] conducted research which established that using additional screws within the intermediate pedicles elevated axial, sagittal, and torsional stiffness by different levels. Therefore, the process could most likely decrease correction loss. Besides, the 3-level fixation supplies a better pull-out strength and therefore theoretically cuts down on the rate of instrumentation failure. However, within this study, there wasn’t any factor in Cobb position restoration and correction loss between two-level fixation and three-level fixation. The reason why might be the following. First of all, the sample size the research wasn’t large enough, which led to a mistake. Next, there was no damage at posterior aspects of thoracolumbar in most patients, therefore the two-level fixation may be sufficient for fracture reduction and stability maintenance. Thirdly, aided with a thoraco-lumbar-sacral brace after surgery, the 2-level fixation could sufficiently keep up with the stability from the hurt segment. Thus, there is no need to deal with every situation of thoracolumbar fracture with intermediate screws. Regardless of caused by this research, the final outcome the three-level fixation boosts the stiffness from the fractured segment can’t be refuted. Using intermediate screws is suggested whenever a patient is by using severe brittle bones, weight problems, apparent injuries of posterior column, etc.
In addition, it’s important to note that no posterolateral bony fusion was performed in both percutaneous surgical procedures or within the traditional open procedure within the study, as several researches demonstrated that posterior pedicle instrumentation without fusion might get comparable results as fixation with fusion [ 16 ].
There’s two primary limitations within the study. First, the research unsuccessful to make use of sagittal index (SI) to explain sagittal deformity, which influenced the precision from the results to some degree. Second, a couple of cases weren’t adopted up lengthy enough. Thus, lengthy-term clinical connection between these cases, for example, correction loss after removing instrumentation, couldn’t be viewed.
Although there are several too little this research, the outcomes still reveal that the final results of both percutaneous and open surgery are acceptable. In contrast to outdoors fixation surgery, the percutaneous fixation surgery has the advantage of causing less operation-related trauma that is advantageous to postoperative rehabilitation. The effectiveness of three-level percutaneous fixation and 2-level percutaneous fixation in treating type A thoracolumbar fractures isn’t considerably different.
Acknowledgments
I must express my gratitude to any or all individuals who helped us throughout the writing of the thesis. I gratefully acknowledge the aid of my supervisor, Professor Zhang Qiulin, that has offered me valuable suggestions within the academic studies. Within the preparation from the thesis, he’s spent enough time studying through each draft and gave me inspiring advice. Without his patient instruction, insightful critique and expert guidance, the conclusion of the thesis will not have been possible.
Compliance with ethical standards




 Hamlets love for ophelia thesis writing
Hamlets love for ophelia thesis writing Writing a thesis flocabulary five things
Writing a thesis flocabulary five things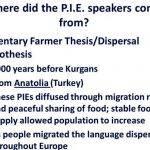 Nomadic warrior thesis versus sedentary farmer thesis writing
Nomadic warrior thesis versus sedentary farmer thesis writing Pericles funeral oration thesis proposal
Pericles funeral oration thesis proposal Table of content for thesis writing
Table of content for thesis writing