A number of factors affect the decision of whether to surgically remove cataracts in the patient with glaucoma.
A cataract is a natural clouding of the lens in the eye. Since the lens is responsible for focusing objects clearly, if the lens is cloudy seeing clearly becomes difficult. Usually the cataract does not interfere with vision initially, and cataracts are not considered an urgent problem. Your ophthalmologist will probably detect a cataract long before you notice it.
A Natural Process
Again, cataracts are a natural process and, thus far, an unavoidable part of aging. As we age the chances of having a cataract increases. For example, it is estimated that in the U.S. less than 4% of men and 10% of women between the ages of 55 and 64 years have visually significant cataracts. Between the ages of 65 and 74 years, 14% of men and 24% of women experience cataracts. The incidence is even higher in those over 75 years old. Because age is a risk factor for glaucoma as well, many patients with glaucoma also have cataracts.
Although all of us will eventually develop cataracts, the good news is that the treatment for cataracts is very successful with the latest surgical techniques. When treatment for a cataract is warranted, it is surgically removed and an artificial lens is put in its place.
Glaucoma, however, damages the optic nerve, the critical structure that transmits the visual signal from the eye to the brain. Unfortunately, in contrast to cataracts, we are not yet able to repair or replace the optic nerve. This important difference affects the management of these two diseases when they co-exist in the same eye.
Tailored Treatment
The ophthalmologist tailors the specific treatment plan for the individual eye to maximize the benefits and minimize the risk to the eye.
The ophthalmologist balances many factors that affect the decision as to when and how aggressively the glaucoma and cataract should be treated, including whether the two diseases should be treated at the same time or separately.
There are a number of options available to glaucoma patients with cataracts, and each situation must be assessed individually. If the cataract does not interfere with the glaucoma patient’s activities significantly then treating the glaucoma and monitoring cataract progression&-but not removing the cataract immediately&-may be an appropriate plan.
Often, the glaucoma can be managed with laser treatment and anti-glaucoma medications. When this is possible, it allows the ophthalmologist to monitor the eye while the cataract worsens.
For patients with mild glaucoma that is stable we might consider surgically removing the cataract and treating the glaucoma with pressure-lowering medications or laser treatments. Cataract surgery alone on an eye with glaucoma will sometimes lower the pressure in the eye.
For patients with more serious glaucoma and the need for cataract surgery, a combination cataract removal and glaucoma filtering procedure can be considered. For patients using multiple anti-glaucoma medications, a combination procedure such as this would be appropriate.
Combination procedures, however, are not for everyone.
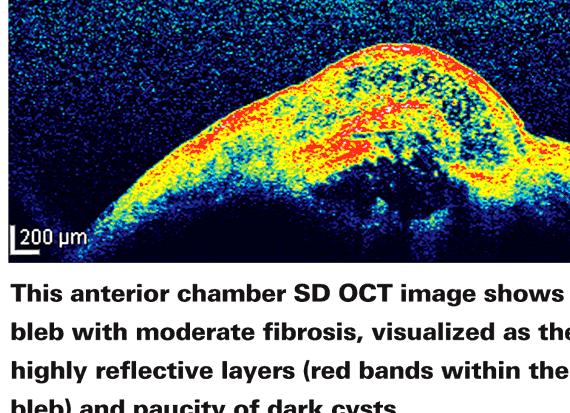
The decision to perform a combination procedure depends on the number of anti-glaucoma medications used, how mature the cataract is, and the state of the glaucoma.
As with any surgery, it is important to discuss the risks and benefits of cataract and combination surgery with your ophthalmologist to determine what is best for you.
—
Article by Andrew G. Iwach, MD. Assistant Clinical Professor of Ophthalmology at the University of California, San Francisco.
Last reviewed on February 13, 2012
Both cataracts and glaucoma can be a natural part of the aging process. Many people over 60 may have both. Otherwise, the two are not associated.
- A cataract is an eye condition where cloudiness, or opacity in the lens, blocks or changes the entry of light, affecting vision.
- Glaucoma is a group of eye diseases that gradually steals sight without warning and often without symptoms. Vision loss is caused by damage to the optic nerve.
Cataracts and glaucoma are both serious conditions that can cause you to lose vision. However, loss of vision due to cataracts can be reversed with surgery. Loss of vision from glaucoma is, as yet, irreversible.
Are those with glaucoma at higher risk to develop cataracts?
Those with glaucoma are usually not at higher risk to develop cataracts. There are exceptions, including those who have glaucoma due to secondary causes such as eye inflammation, eye trauma, or steroids. Also at higher risk are those with developmental conditions, such as congenital rubella, which can cause glaucoma, cataracts, or sometimes both. Both eye conditions are also more common with age, which is why many who have one disease may develop the other.
Can surgery restore vision loss from a cataract?
Unlike vision loss from glaucoma, cataract vision loss can often be regained. In most cases of cataract surgery, the cloudy lens of the eyes is removed and replaced with a clear plastic lens (called an intraocular lens implant).
The cloudy lens is removed.
The process of removing a cataract is called extracapsular lens extraction. After this process, an outer membrane lens capsule often remains. This membrane can slowly thicken and cloud vision. A laser procedure called a capsulotomy can open this membrane, restoring vision without the standard cutting procedure.
When is cataract surgery needed?
Cataract surgery is suggested when a person’s vision has declined to the point where it interferes with their usual daily tasks.
If a cataract develops in a part of the eye lens where it does not affect vision, cataract surgery may never be needed.
How will cataract surgery affect the glaucoma?
Cataract surgery can cause a change in the eye’s pressure. This change may be short-term or permanent. In general, it is not possible to predict whether the IOP will rise, fall or stay the same after cataract surgery.
Sharp increases in eye pressure are called &”pressure spikes&” and sometimes occur in patients after cataract surgery. Often these pressure spikes are short-term and can be treated with medicines.
If both glaucoma surgery and cataract surgery are needed, can the two procedures be combined?
The first priority is to control the person’s glaucoma. A person may have a glaucoma procedure followed by cataract surgery, or have both surgeries done at the same time. The specific approach will depend on the medical needs of the person with glaucoma.
How do cataracts and glaucoma medicines interact?
Those who have glaucoma and use adrenergic agonist medicines, such as epinephrine or Propine, may notice an increase in glare, if they have a cataract. This is because these eye drops may make the pupil larger and can expose the cataract to more light.
Others who use miotic eye drops, such as pilocarpine or carbachol, for intraocular pressure (IOP) control may find their vision lowered by the glaucoma medicines. These medicines tend to shrink the pupil, which lowers the amount of light entering the eyes. Since cataracts may already be clouding vision, this may make vision worse.
Those who have either of these problems may wish to talk to their doctor about possible treatment options, such as other medicines, laser treatment, or surgery.
Can medicine treat cataracts?
There are no current medicines that have been proven to be helpful in the treatment of cataracts.
Special thanks to Michael Sakamoto, MD for contributing to this article.
Last reviewed on May 02, 2011




 Hybrid solar cell thesis writing
Hybrid solar cell thesis writing Social media marketing communication thesis proposals
Social media marketing communication thesis proposals Sample title for thesis proposal
Sample title for thesis proposal Caution thesis writing in progress phd comics door
Caution thesis writing in progress phd comics door Thesis writing services in malaysia flight
Thesis writing services in malaysia flight